Http://www.hoffmanpr.com/cgi-script/csarticles/articles/000001/000153.htm
Press Release: Healthy Children, Healthy Futures: INMED’s Public-Private Partnership Initiative Improves the Health and Lives of Brazil’s Children (Joyce Capelli or Linda Pfeiffer of INMED, will be available for interviews in São Paulo on April16, 17 and 18. Please call Nils Hoffman or Liliana Hisas to schedule time. Thad Jackson orSuzanne Wilcox of INMED will be available for int
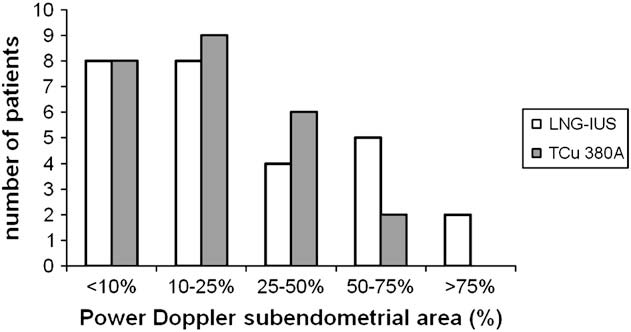 The demographic characteristics, pulsatility
index (PI), and resistance index (RI) of the 52
insertion) in the pulsatility index (PI),
women before IUD insertion: mean (SEM).
The demographic characteristics, pulsatility
index (PI), and resistance index (RI) of the 52
insertion) in the pulsatility index (PI),
women before IUD insertion: mean (SEM).