Doi:10.1016/j.juro.2007.03.132
Effect of Statin Therapy on Early Return of Potency After Nerve Sparing Radical Retropubic Prostatectomy Sung Kyu Hong, Byung Kyu Han, Seong Jin Jeong, Seok-Soo Byun and Sang Eun Lee* From the Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea Purpose: We prospectively investigated whether postoperative statin use would contribute to earlier recovery of er
 Available online at www.sciencedirect.com
Intra-articularly applied pulsed radiofrequency can reduce chronic
knee pain in patients with osteoarthritis
Haktan Karaman , Adnan Tu¨fek , Go¨nu¨l O
a Department of Anesthesiology, Pain Management Center, Dicle University, Diyarbakir, Turkey
b Department of Anesthesiology, Dicle University, Diyarbakir, Turkey
c Diyarbakir Vocational Higher School, Department of Technique, Dicle University, Diyarbakir, Turkey
d Department of Anesthesiology, Diyarbakir Education and Research Hospital, Diyarbakir, Turkey
Received October 4, 2010; accepted February 19, 2011
Background: Osteoarthritis (OA) is the most widespread chronic joint disease worldwide. Symptomatic knee OA is observed in approximately12% of individuals more than 60 years of age. Conservative treatments models may not be effective always, and that some of them have seriousadverse effects that prompted the researchers to research different treatment methods. In this study, we investigated short- and mid-termeffectiveness of intra-articular pulsed radiofrequency (PRF) applied in patients with chronic knee pain due to OA.
Available online at www.sciencedirect.com
Intra-articularly applied pulsed radiofrequency can reduce chronic
knee pain in patients with osteoarthritis
Haktan Karaman , Adnan Tu¨fek , Go¨nu¨l O
a Department of Anesthesiology, Pain Management Center, Dicle University, Diyarbakir, Turkey
b Department of Anesthesiology, Dicle University, Diyarbakir, Turkey
c Diyarbakir Vocational Higher School, Department of Technique, Dicle University, Diyarbakir, Turkey
d Department of Anesthesiology, Diyarbakir Education and Research Hospital, Diyarbakir, Turkey
Received October 4, 2010; accepted February 19, 2011
Background: Osteoarthritis (OA) is the most widespread chronic joint disease worldwide. Symptomatic knee OA is observed in approximately12% of individuals more than 60 years of age. Conservative treatments models may not be effective always, and that some of them have seriousadverse effects that prompted the researchers to research different treatment methods. In this study, we investigated short- and mid-termeffectiveness of intra-articular pulsed radiofrequency (PRF) applied in patients with chronic knee pain due to OA.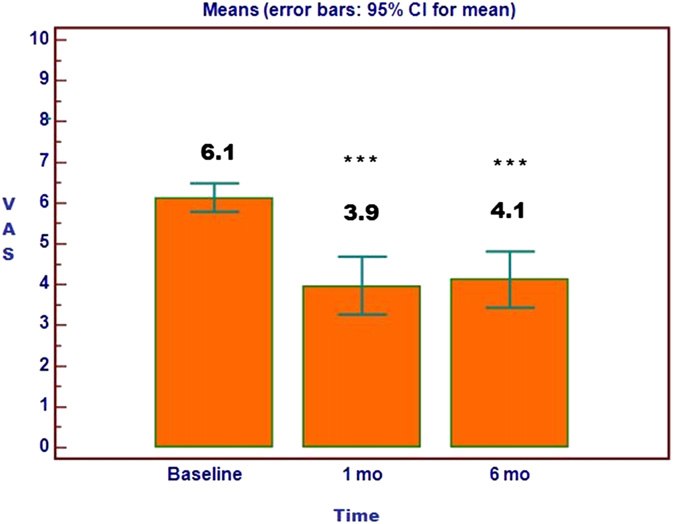 H. Karaman et al. / Journal of the Chinese Medical Association 74 (2011) 336e340
suggestions to rest for the 1st day and then engage in their
Demographic characteristics of study patients
The pain of the patients was evaluated by a 10-cm VAS. In
this scale, “0” identifies the situation where no pain exists and
“10” identifies the most severe pain that can be imagined.
H. Karaman et al. / Journal of the Chinese Medical Association 74 (2011) 336e340
suggestions to rest for the 1st day and then engage in their
Demographic characteristics of study patients
The pain of the patients was evaluated by a 10-cm VAS. In
this scale, “0” identifies the situation where no pain exists and
“10” identifies the most severe pain that can be imagined.